It’s a fortnight since we got back from a “holiday of a lifetime” – long haul flights, theme parks, cruise ships and Caribbean islands. It was long planned and much anticipated and three of the family had the “best time ever.” My own fun was a little limited by my first ever experience of the flu and although I still had a great time my mood since returning has been a little flat. Post viral fatigue on a background of demyelination is enough to keep you in your bed for a week it seems!
But the weekend brought an improvement, gave me time to catch up with some friends, and it also brought the sunshine and things look rosier. I really like spring and it’s the five year anniversary of my diagnosis this week – time to compare what I thought my life might be like at this point to how it actually is.
As readers of previous entries might know, as well as fear and uncertainty, a prominent emotion at the time of diagnosis was relief that what I was experiencing was “real” and that it had an explanation. I still feel this now. I have a diagnosis that people recognise, I qualify for various “treats” such as a blue badge and my new shiny radar key, and I generally understand the course of my own particular version of this illness so that when I do take to my bed I am (at least 75%) confident that at some point I will be able to get back out again. And the darkest fears that kept me awake at night half a decade ago have not come to pass. I can still ride on (tame) rollercoasters, I can still drive huge American cars, I can still walk around Diagon Alley with wonderment instead of pain and, even if I can’t scuba dive, I can still watch my family do it from a lovely boat floating on a turquoise ocean. I am a lucky woman.
Day to day I try to remember how lucky I am but, inevitably, the positive feelings can be buried under the pressure of being good enough at my demanding job whilst giving enough time to children who need more emotional input than ever. The anxiety of a never-ending to-do list occasionally makes me want to hide under a blanket and on those days I don’t feel thankful or grateful. But I also spend a period of time each year trying to focus on the things each day that I have to be thankful for. Because I am a chronic over-sharer I tend to outline these on Facebook which I worry may come across as a little smug, but one thing I am trying to cross off the to-do list is “worrying what other people think of me.” It helps me, it is appreciated by many people I love, and it may inspire people to find their own good bits in stressful, frenetic and occasionally troubled lives.
The inspiration for this year’s positivity comes from two places. Firstly my choir. I love my choir. I am almost certainly the least tuneful member of it but no-one is mean enough to mention it. And we sing a great warm-up song with the lyrics “love lifted me.” Every time we sing it it makes me think of all the ways that love has lifted me up when illness/stress/exams/worries about children, money, relationships etc has laid me a little low. The love of other people and the ways in which they show it rarely fails to lift me but perhaps I don’t always acknowledge how grateful I am for that. So my first tag this month will be #loveliftedme.
And the second comes from another place where I feel calm and mindful and that is the Church where my husband and children are members. I am not a Christian; I don’t have a religious faith. My husband has faith but was disillusioned by the narrowness, intolerance and small-mindedness of the Church in which he was raised so didn’t attend for many years. But he has found a spiritual home in the place he now attends, the children subsequently chose to be baptised there and I like to go along to sing, see people, and listen to the sermons that preach messages of love, inclusion and self-challenge. A recent sermon by a visiting Minister discussed the concept of “thanksliving” – of living each day purposefully acknowledging your blessings and actively showing your thanks for what you have. This could be through daily acts of kindness, charitable works and volunteering, or simple recognition of what you have to be thankful for. References to this on Google are almost universally faith based but there is no reason why it can’t be applied to a secular setting and this is my new challenge.
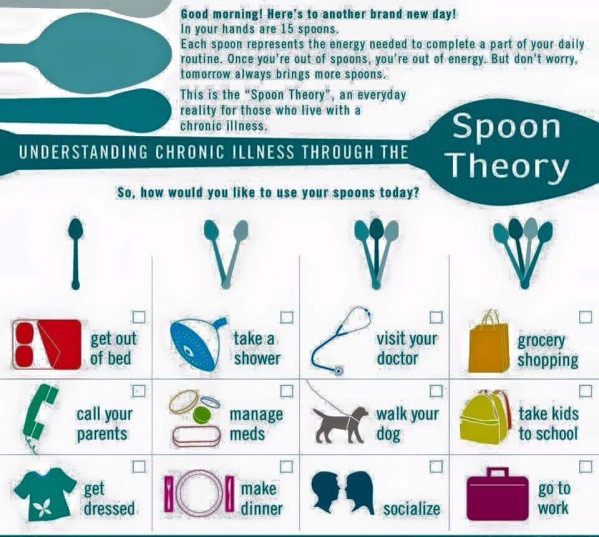
I face the same difficulties as any working mother. I am tired, my children are over-scheduled (although happy to be so it seems), I communicate with my husband mostly via text arranging who needs to do what when, I fail to give any of them five portions of fruit and veg a day and one of my son’s classmates last week told him the world book day costume didn’t look like I had “put much effort in.” (!!!) I haven’t had my hair cut in a VERY long time and I can’t remember the last time the windows were cleaned. I don’t give enough energy to my work and I wish I had more energy available to see my friends and family. And I have a (currently) incurable and progressive neurological condition which, on some days, makes all of the above seem less like a quirky list of shortcomings and more like an overwhelming ledger of how I am failing.
So I will do what I need to do to focus away from the malfunctions and towards the loveliness. Away from the irritation and more to the blessings. I hope it doesn’t annoy those of you who see it, but if it does I apologise a little but it is helping me a lot!
#loveliftedme #thanksliving